Causes
Several types of source can cause rhinosinusitis. The problems can last only a short time, termed acute rhinosinusitis, or they can last for months of even years, called chronic rhinosinusitis. Different causes are susceptible to different treatments.
Contents
Environmental
The environment contains extensive sources of nose and sinus irritants. Some of these can form biofilms, protective meshes that prevent the pathogens from being destroyed.
Substances
Substances can directly interfere with sinus function, or trigger harmful bodily response
- Viruses such as the common cold do not respond to antibacterial therapy. They usually result only in acute rhinosinusitis, however complications can lead to chronic rhinosinusitis.
- Bacteria can cause sinus symptoms. Particularly implicated in chronic rhinosinusitis is Staphylococcus aureus [1]. Bacteria can be treated with antibacterial agents.
- Molds.
- Allergens cause temporary swelling of the nose and sinuses. These can be relieved with antihistamines. [2]
- Substances in food could contribute to rhinosinusitis, whether through allergic or non-allergic reactions.
- Common food allergies that can induce rhinosinusitis include dairy, peanuts, tree nuts, wheat, and other grains. An elimination diet, in which the person eats a simple diet, can reveal possible allergens.
- Alcohol can potentially aggravate sinus issues.
- Preservatives and other additives are believed by some people to affect sinuses.
Weather
Weather conditions can cause serious sinus issues. In particular, extremely high or low humidity and extremely cold or hot weather can cause problems. Sudden changes in atmospheric pressure, such as before a storm, can also aggravate problems.
- High temperature, and dew point could contribute to sinus symptoms.
- Low visibility could indicate weather conducive to sinus symptoms.
- High wind could rapidly introduce different weather conditions, affecting sinus symptoms.
- The relationships between weather and sinus symptoms can be quite complex. At times, a weather component can track strongly with symptoms, at other times strongly against.
Variable
Conditions that vary from person to person, or for one person at different times, can affect sinus symptoms.
- Time of day.
- Sinus symptoms can improve or worsen throughout the day. This can depend on weather, alertness, and other factors. Symptoms often systematically reflect the time of day.
- Stress. Various environmental stressors, from loud noises to busy work lives, can contribute to sinus problems. Sometimes stress relief can reduce rhinosinusitis.
- Glasses. Wearing spectacles applies additional pressure on the sinuses that can cause problems.
Biological
People are born with a set of genetic coding that can predispose the person towards rhinosinusitis. Additional biological developments throughout the course of life can cause sinus issues.
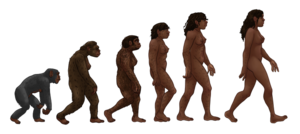
Humans evolved such that an upright posture and a large forebrain apply unusual pressures on the sinuses. [5] This development may have happened too fast for the sinuses to rebalance appropriately, explaining the large number and severity of sinus issues.
Traditionally, blockage of maxillary ostia (sinus openings into the nose) have been seen as leading to congestion and sinusitis. The maxillary ostia are located high up the sinuses, preventing gravity from clearing the sinuses, and requiring the cilia (clearing hairs) to do more work. This results in less effective clearance. More recent research has found that blockage of the nostrils can also lead to sinusitis. As air flows more freely through the nose and sinuses, it assists in clearing mucus.
It is hypothesized that alterations in mucociliary clearance, abnormalities in the sinonasal epithelial cell barrier, and tissue remodeling all contribute to the chronic inflammatory and tissue-deforming processes characteristic of CRS. [6]
Complex microbial communities have co-evolved with our species. At any one time, an individual can host 10 to 100 trillion microorganisms, outnumbering human cells by at least a factor of 10. Bacterial communities have been demonstrated on the mucosa of the entire respiratory tract, with the highest concentrations being found in the upper respiratory tract... There is some recent evidence that mucosal inflammation in the paranasal sinuses is associated with a decreased diversity of the local bacterial communities. Particular microbial species known as “keystone species” may have an exceptionally large impact on the ecosystem's function and health. [7]
Biofilms
Biofilms are three-dimensional networks that protect and nourish microbes. This includes healthy and pathogenic microbes.
Multiple bacterial and fungal species can live in a single biofilm. A biofilm also allows the organisms to have metabolic cooperation that enhances efficiency, quorum sensing systems that control growth and an enlarged gene pool with more effective DNA sharing capabilities.... However, in the context of CRS there are several possible mechanisms by which biofilms may be pro-inflammatory including the release of planktonic organisms and the production of superantigens, which can cause ciliary dysfunction and inhibition of mucociliary clearance. [8]
Below the surface, problems can make surgical and medical responses ineffective.
Intra-epithelial microorganisms have also been identified in CRS patients, including S. aureus. Microcolonies have also been identified in the interstitium just below the epithelial layer. As these colonies do not initiate a host immune response, they may act as a source for ongoing inflammation following medical and surgical treatment. It is likely that these factors in combination with host immune system responses and disrupted epithelial lining play a role in the pathogenesis of CRS. [9]
Endotyping
New research investigates the specific biological mechanisms underlying cases of chronic rhinosinustis. [10] This process of endotyping includes particular molecules and cells, such as T helper cells.
Experts agree that the elevation of these inflammatory endpoints may be the result of maladaptive immune signaling, triggered by impaired mucociliary function and epithelial cell barrier breakdown. [11]
CRS is due to dysregulated immunologic responses to external stimuli, which induces inflammatory mediators. [12]
Variations
Anatomical variations are abundant. Just as each person has a different fingerprint or face, each person has different sinuses.
- Small or otherwise malformed sinuses or nose.
- Some people argue that autistic personality types are associated with a particular frontal sinus problem. [13]
- Thicker mucus is more viscous and difficult to clear compared to thin mucus. This can change from individual to individual, and over time. In particular, various illnesses can temporarily affect the consistency of mucus.
- Weak immune system.
- Polyps.
- Deviated septum.
- Thyroid problems could cause imbalances in signaling in the body.
- Some people have poorly functioning mucus membranes.
- Cases of rhinosinusitis often fall into different categories of pathogenic cause. [14]
- An airway protein (surfactant protein A) respond to disease-causing bacteria, and also alter inflammation levels. [15]